
This annual report presents information and statistics that serve as indicators of quality for our mental health services. Active monitoring of services is vital to ensuring New Zealanders are receiving quality mental health care.
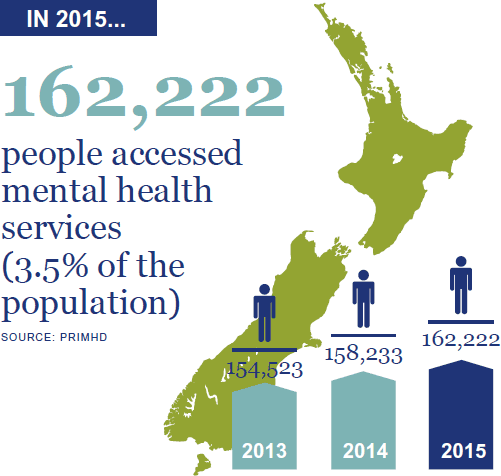
The focus of this year’s report is on the transformational journey that mental health care in New Zealand is undergoing. In 2015 a record number of people accessed specialist mental health and addiction services. This increase is consistent with international trends, and has occurred in the context of population growth, improved non-governmental organisation reporting, growing social awareness and increasingly open discussion of mental health issues.
More New Zealanders are seeking and receiving mental health care, which is positive. But services are experiencing increasing pressure. We must continue to ensure that services are best placed to respond to the changing needs of the populations they serve.
This report is divided into three main sections.
- Context – an overview of the legislative and service delivery contexts in which the Office operates.
- Activities for 2015 – the work carried out by the Office in 2015.
- Ensuring service quality – statistical information on the use of compulsory mental health assessment and treatment, family/whānau consultation, seclusion, electroconvulsive therapy, reportable deaths, suicide and opioid substitution treatment during 2015.
Performance

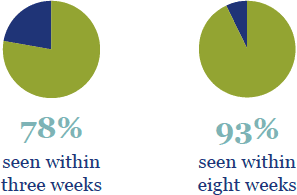
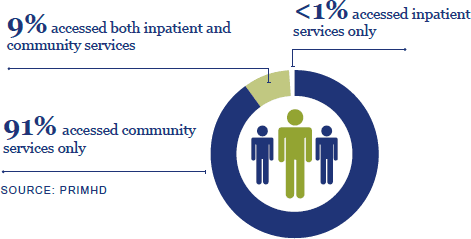
Access
Compulsory assessment and treatment under the Mental Health Act 1992

1. This relates to community treatment orders (section 29 of the Act). Māori were 3.3 times more likely than non-Māori to be subject to inpatient treatment orders (section 30).

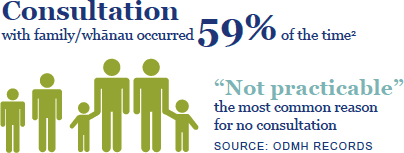
2. Across all assessment and treatment events (sections 10, 12, 14 and 76, and release from the Act).
Seclusion3 in mental health services has been declining since 2009
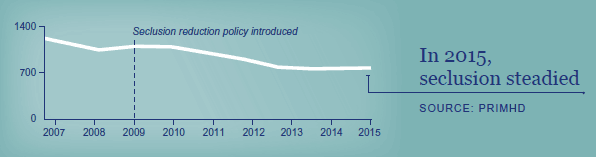
3. Seclusion is ‘where a consumer is placed alone in a room or area, at any time and for any duration, from which they cannot freely exit’ (Standards New Zealand 2008a).
